What are the functions of human kidney? Information on urine formation an d the processes occur in human kidney.
The major role of the kidney is the formation of urine. However, the kidney also plays important roles in other body activities. It influences the formation of red blood cells, stimulates the formation of steroids, helps control blood pressure, and affects many of the substances involved in metabolism.
Urine Formation:
The first and main step in urine formation is glomerular filtration. In this process, the blood’s pressure forces water and other small molecules in the blood through the walls of the glomerular capillaries into the glomerular capsule and nephron tubule. Blood cells and proteins do not pass through the capillary walls and remain in the blood. In an average-sized young adult, the amount of filtrate formed in the nephrons is about 4.5 ounces (130 ml) a minute, or about 10.5 quarts (187 liters) a day, representing about 1/5 of the total amount of blood plasma entering the glomerular capillaries.
After the filtrate flows from the glomerulus to the tubule, certain wastes are added to it by another process, called tubular secretion. Secretion is accomplished mainly by cells of proximal segment, which actively transfer numerous organic acids and bases from the blood into the tubule. Apparently only two major secretory transport mechanisms are involved, one for acids and one for bases. In addition to organic wastes, hydrogen ions and ammonia are secreted throughout the length of the tubule, and potassium is secreted in the distal segment.
Source : pixabay.com
The reabsorption of most of the materials from the filtrate back into the blood occurs in the proximal segment of the nephron tubule. In this segment, about 80% of the water and salts are reabsorbed and from 95% to 99.9% of the sugars, amino acids, and other substances used in metabolism are reabsorbed. Wastes, such as urea and creatinine, remain in the tubular fluid. As the filtrate passes through the distal segment of the tubule, additional salts and water are reabsorbed, reducing the volume and concentration of the urine to its normal levels.
Both secretory and reabsorptive processes of the kidney vary according to the body’s need to eliminate excess materials and conserve essential materials. These processes almost exclusively involve salts and water.
Sodium and Chloride Ions:
Sodium and chloride ions are extensively reabsorbed in the straight ascending portion of the loop of Henle. Where the tubule passes through the medulla, the salts tend to accumulate in the medullary fluid, making it highly concentrated. Additional sodium and chloride ions are reabsorbed in the distal convoluted segment and also possibly in the connecting segment. Reabsorption in these segments is enhanced by the presence of steroids, particularly aldosterone, which are secreted by the adrenal glands.
Aldosterone is secreted when the body’s level of sodium falls below normal. The secretion takes place through a complex mechanism involving both a liberation of the hormone renin from the kidney itself and a secretion of other agents from the brain or pituitary gland. When there is an excess of sodium chloride in the body, the secretion of aldosterone diminishes, the reabsorption of salt is less complete, and more salt is excreted.
In addition to aldosterone and other steroids, other factors influence the excretion of sodium and chloride. One such factor is the amount of filtrate formed. An increase in filtrate increases the excretion of sodium and chloride ions while a decrease in the amount of filtrate decreases their excretion. An obscure endocrine system, which is particularly active in the presence of a great excess of salt, may substantially depress the reabsorption of sodium and chloride ions in both the proximal and distal segments of the nephron tubule.
Potassium Ions:
Some reabsorption of potassium ions occurs in the straight portion of the distal segment while the most extensive secretion of potassium ions occurs in the convoluted portion of the distal segment and in succeeding segments of the tubule. The secretory process consists of an ion-for-ion exchange of potassium (from the blood) for sodium (from the tubular fluid), and it is stimulated both by the concentration of potassium ions in the blood and by the secretion of adrenal and similar steroids.
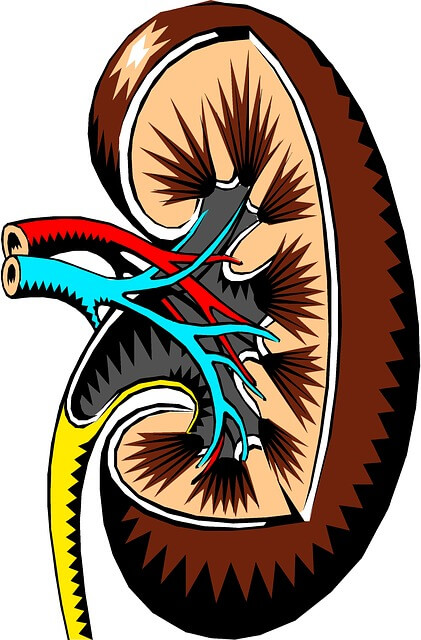
Source : pixabay.com
Acid:
The excretion of acid in the urine cannot occur until bicarbonate ions, a base, are first removed from the glomerular filtrate. Removal of bicarbonate is accomplished by the reabsorption of bicarbonate itself and by the secretion of hydrogen ions into the tubule. This latter process is followed by a breakdown of bicarbonate ions into carbon dioxide and the diffusion of this gas into the bloodstream. A strongly acidic urine is formed in the distal convoluted segment and subsequent segments by an exchange of sodium ions for hydrogen ions that are generated from water by the tubule cells. Since the most acidic urine the kidney is capable of forming has a pH of about 4.5-5.0—which represents relatively few free hydrogen ions—urinary buffers, notably phosphates, are needed to combine with hydrogen ions and thus make possible the elimination of significant amounts of acid.
Ammonia:
The cells of nephron tubules continually synthesize ammonia through the action of numerous enzymes on amino acids. The ammonia readily passes through the cells and accumulates in the urine, reacting with the hydrogen ions there to create ammonium ions. Thus, ammonia facilitates the excretion of acid from the body by acting as a buffer. In acidosis, a condition in which the body fluids become too acidic, the tubule cells greatly increase their output of ammonia to increase the excretion of acids. Although all parts of the tubule can secrete ammonia, secretion appears to be greatest in the distal convoluted segment and lower portions, where the acidity of the tubule fluid is greatest.
Water:
Since the amount of watery filtrate formed by the nephrons amounts to about 10.5 quarts per day for an average adult, a large amount of water must be reabsorbed from the filtrate into body fluids to prevent excessive loss of water through urination. Reabsorption of water is stimulated by the presence of the hormone vasopressin, which causes the portion of the tubule from the distal segment downward to become highly permeable to water.
As a result, the water in the tubular fluid moves by osmosis into the concentrated fluid outside the tubule and the volume of fluid inside the tubule shrinks until its concentration equals that of fluid outside. Further reabsorption of water takes place in the collecting ducts that pass through the medulla. The fluid in the tissue of the medulla contains a higher concentration of sodium ions, chloride ions, and urea than the fluid entering the ducts. Consequently water moves by osmosis through the walls of the duct until its concentration balances that of the medullary fluids.
If the hormone vasopressin, which is secreted by the posterior pituitary gland, is absent from the blood, as in certain diseases, the dilute fluid continues to the bladder, and the person excretes large amounts of a very dilute urine.
Other Kidney Functions
Red Cell Formation:
When there is a loss of blood or a deficiency of oxygen in the blood, the kidneys respond by liberating into the bloodstream a protein, erythropoietin, which stimulates the bone marrow to increase its production of red blood cells (erythrocytes). It is not known how erythropoietin is produced or exactly how it acts on the marrow.
Stimulation of Steroid Production:
In some states of stress, notably when excessive amounts of fluid are lost from the body, the kidneys release the enzyme renin into the blood, where it reacts with other proteins to produce angiotensin. Angiotensin acts as a potent stimulator of the adrenal glands to secrete the steroids aldosterone and corticosterone. Angiotensin also directly affects salt excretion and tends to increase the blood pressure; however, it is not known whether these are normal functions of the protein.
Source : pixabay.com
Blood Pressure:
An increase in blood pressure is commonly seen in many kidney diseases, and it is believed that this increase may be caused by certain substances released from the kidney. Renin and angiotensin are not necessarily involved in the blood pressure rise, and the cause of this phenomenon is not fully understood.
Metabolic Substances:
The kidney rivals the liver in its effect on many of the substances involved in metabolism. For example, the kidneys may remove, but not excrete, large amounts of citric acid as well as fructose and lactic acid from the blood. They may also convert numerous wastes, such as benzoic acid, into forms that can be secreted into the nephron tubule by coupling them with the amino acid glycine or similar agents.