What is the definition of white blood cell? Information about the structure and functions of white blood cells.
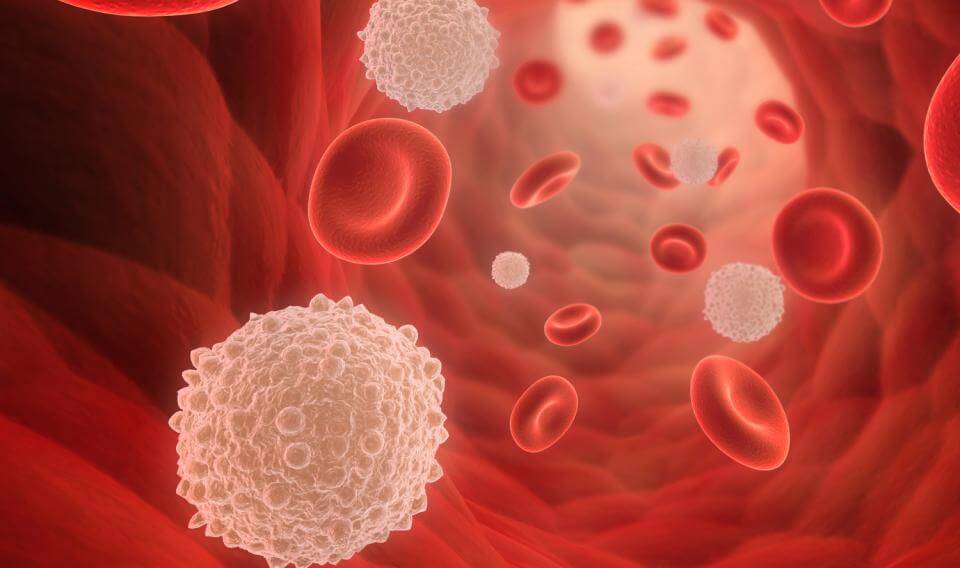
White Blood Cells; The white blood cells, or leukocytes, differ from the red blood cells in several important ways. Unlike red cells, they are complete cells, possessing a nucleus and varying amounts of granules in their cytoplasm. They are also larger than red cells, measuring from 10 to 20 microns in diameter. In addition, white blood cells are capable of moving about independently and are not merely carried by the bloodstream. They can also move out of the bloodstream, squeezing between the cells that line the walls of the blood vessels.
Their method of locomotion is similar to that of one-celled organisms known as amoebas. There are many fewer white blood cells than red cells, although the normal number of white cells varies according to age. In normal adults there are about 7,000 white blood cells per cubic millimeter of blood. In a newborn infant, there are more than 15,000 and often from 25,000 to 30,000. However, the white cell count drops quickly on the third or fourth day of life and then fluctuates from 9,000 to 14,000 until it drops to adult levels at puberty.
The most important members of the white cell family are the granulocytes, lymphocytes, and monocytes. The granulocytes, which are formed in the bone marrow, are further subdivided into three groups—neutrophils, eosinophils, and basophils—on the basis of their affinity for certain dyes. The lymphocytes and monocytes are formed mostly in the lymph nodes and spleen. The approximate distribution of the white cells is as follows: granulocytes, 70%; lymphocytes, 20%; and monocytes, 10%.
The white blood cells serve to protect the body against infection by two methods. In phagocytosis (literally meaning “cell eating”), the cells engulf and digest bacteria, cellular debris, old cells, and other foreign bodies. This function is largely performed by the more mobile white blood cells—the neutrophils, eosinophils, and the monocytes. The second method of defense is the production of antibodies. The lymphocytes and plasma cells (cells that enter the blood only when infection occurs) lead in this function.
Whenever infective matter penetrates the body tissues—for example, when a boil develops on the neck—the granulocytes move swiftly into the area, collecting around the bacteria and destroying them. During this process many of the granulocytes degenerate, and their remnants appear in the pus draining from the infection. As the second line of defense, the monocytes attack. These white blood cells have the ability to engulf particles other than bacteria. The lymphocytes, the third line, are activated by contact with the infective agent, and they promote the production of antibodies that later attack and destroy residual bacteria.
In acute infections, such as appendicitis, pneumonia, and meningitis, the granulocytes play the strongest defense role. In indolent infections (ones that progress slowly) such as tuberculosis, syphilis, and malaria, the monocytes dominate the defense. In other infections, including infectious mononucleosis, German measles, and most other virus infections, the lymphocytes are most active. In all infections, however, the various activities of the white blood cells are nearly always self-limited. Once the infective agent is gone, the reaction gradually ends.
mavi