Embark on a fascinating exploration of the history of surgery. Trace its evolution from ancient civilizations to the cutting-edge techniques of today, witnessing the remarkable milestones, innovations, and contributions that have shaped the field of medical science.

Although surgery was practiced in ancient times, modern surgery may be said to begin with the rapid progress made in the last quarter of the 19th century, following the introduction of anesthesia and antisepsis. However, important steps in the development of modern surgery occurred prior to the late 19th century. These steps included the raising of the educational standards and social status of the surgeon, the development of a scientific approach to surgery, and the introduction of a number of technical innovations and achievements, such as the effective control of bleeding.
Early Surgery.
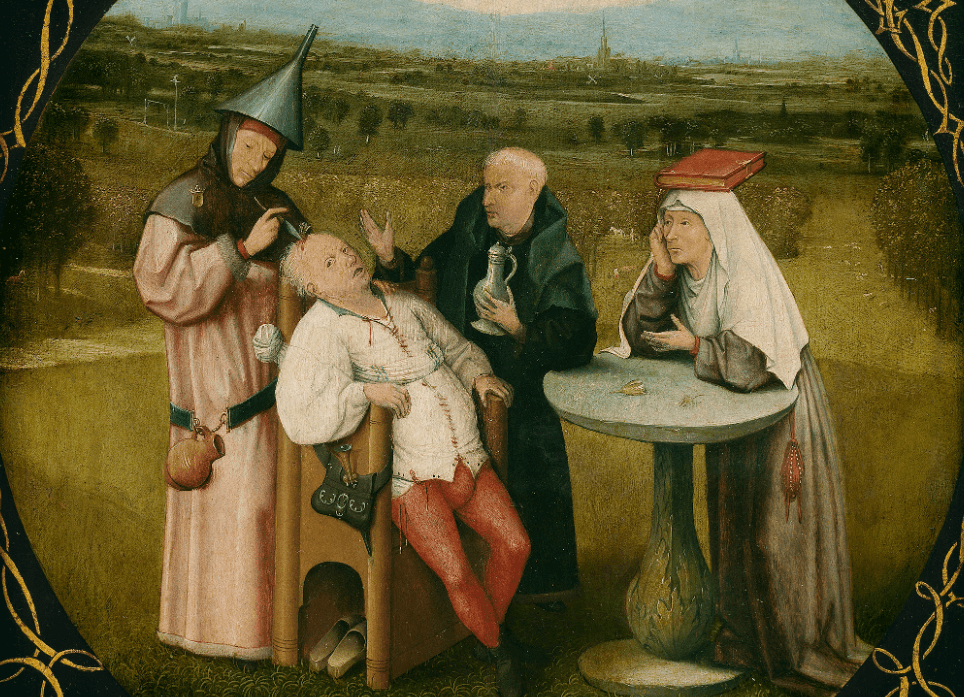
Paleopathology, the study of disease in fossil plants and animals, indicates that virtually all major categories of disease are as old as man or even older. The surgical treatment of disease almost certainly predates the invention of writing; thus there are no written records of the earliest surgical operations. However, prehistoric skulls reveal that trepanning, or the removal of parts of bone from the skull, was performed in many primitive societies. It is doubtful, though, that the operation was undertaken for therapeutic reasons. It may have been performed as a part of magico-religious ceremonies.
The Edwin Smith Papyrus, a part of an Egyptian manuscript written in the 17th century b. c. and discovered by Edwin Smith in the mid-1800’s, is the oldest known Egyptian medical document and the only early document dealing exclusively with surgery. It is actually a copy of a text originally written about 2500 b. c. The surviving fragment of the manuscript contains descriptions of about 50 cases of varying severity, many of which are head injuries. Each description follows the same pattern: the problem is identified, an examination is outlined, and one of three classifications of treatment is recommended. The ailment may be treated, “contended with,” or not treated at all. The anatomical descriptions in the papyrus are precise and objective. Especially noteworthy is the absence of magical or religious elements that are prominent in other Egyptian medical writings.
The complete absence of Mesopotamian surgical writings suggests that the practice of surgery there may have been discouraged by the harsh penalties for unsuccessful treatment, as specified, for example, in the Babylonian legal codes. In China, until the 20th century, and in Japan, until the time of the first Western contacts, surgery was generally neglected. Religious and philosophical dogmas were averse to anatomical dissection and operations in which blood was shed. The scarcity of surgical documents from these ancient civilizations probably means that necessary restorative procedures, such as the care of wounds and the setting of fractures, were avoided by the regular medical practitioners and were relegated to others.
Hindu surgery, on the other hand, was highly developed, as shown by the major surgical text, the Susruta Samhita, which was written sometime between the 6th century b. c. and the 6th century a. d. This work treats surgery as the first and most important branch of medical science. Although the anatomical descriptions are vague, there are precisely detailed accounts of the examination of patients and the prognoses of diseases. More than 100 instruments, the majority of which are blunt rather than cutting, are also mentioned. Some degree of anesthesia was obtained by giving patients alcohol and narcotics. Among the various operations performed were the extraction of urinary bladder stones and plastic surgery. Replacing a destroyed nose was ac-coniplished by transplanting a flap of skin from elsewhere on the patient’s body.
Greek and Roman Surgery.
In the 5th century b. c., Greek medicine, along with other aspects of Greek civilization, enjoyed a remarkable flowering. Over 70 medical treatises written around that time were gathered together several centuries later by Alexandrian scholars who attributed them to the Greek physician Hippocrates. Today it is generally agreed that these works were composed by many different authors who, like the other physicians at the time, seem to have practiced both medicine and surgery. Although they regard surgery as a last resort, these treatises describe surgical procedures for treating head injuries, fractures, dislocations, hemorrhoids, ulcers, fistulas, and wounds. In contrast to the vague anatomical descriptions found in other medical treatises, the surgical anatomy is accurate and precise. The description and treatment of dislocations of the hip and shoulder and congenital clubfoot are excellent even by modern standards.
During the centuries following the decline of classical Greece, the major scientific as well as political center was Alexandria, Egypt. For the first time in history, large-scale human dissection was legalized, and as a result many anatomical discoveries were made. Only a few fragments of the works of the chief anatomists of this period— Herophilus and Erasistratus—are extant. However, Celsus, a Latin author of the 1st century a. d., summed up the progress of surgery during the 500 years after the writing of the Hippo-cratic treatises. In general, surgery was less conservative during this time than during the Hip-pocratic period. Operations not mentioned in the earlier treatises, such as the extraction of urinary bladder stones and operations to treat hernias, are detailed by Celsus. Other notable achievements recorded by Celsus are eye surgery and the use of ligatures to control bleeding. Celsus considered surgery, together with dietary measures and the use of drugs, as one type of therapy available to the doctor. He did not separate surgeons from physicians in either theory or practice.
Galen, the Greek physician who lived during the 2d century a. d., is one of the most famous doctors of antiquity. He is remembered chiefly for his views on physiology and pathology, which dominated medical thought for more than 1,500 years. However, Galen also practiced surgery, and his writings on the ailments that were considered to be surgical diseases—tumors, inflammations, abscesses, and wounds—acquired dogmatic authority during the centuries succeeding Galen’s death.
Byzantine and Arabic Surgery.
After the death of Galen, medical authorities, especially in the Byzantine Empire, wrote long compilations of earlier medical knowledge. The last of these encyclopedic authors, Paul of Aegina, who lived during the 7th century, summarized the medical works of Hippocrates, Galen, and others. Paul’s encyclopedia, in turn, was the source of much Arabic and late Western medieval surgery.
Paul’s surgical writings included observations from his own practice, including descriptions of the extraction of arrows lodged near large blood vessels or in the chest. Some procedures, which he apparently derived from surgeons whose works are lost, were definite advances and represent the high point of ancient surgery. Examples of such procedures are tracheotomies and operations to treat aneurysms (abnormal dilations of blood vessels) in the extremities. In other aspects, Byzantine surgery was cruder and crueler than earlier techniques. For example, there was much emphasis on the use of the hot cautery and the encouragement of the formation of pus in wounds.
Surgical knowledge stagnated during the centuries when the culture of antiquity passed over to the Arabic-speaking world. The Islamic religion inhibited anatomical research and any therapy involving bloodshed. Surgery took on the status of a lowly occupation, distinct from medicine and practiced by uneducated craftsmen in cases where it could not be avoided. The only Arabic author to write a separate treatise on surgery was Albucasis, a native of Muslim Spain who lived during the 11th century. Albucasis relied heavily on the surgical writings of Paul of Aegina, and he dealt extensively with eye diseases, frequent ailments in the Muslim lands. His text was exceptional for its many illustrations of surgical instruments, although cauterization was preferred to the knife in the treatment of a variety of diseases. Although his influence on his own culture was slight, Albucasis’ text, in a Latin translation, served as a basis for western European surgical authors in the late Middle Ages and later.
Medieval Europe.
Little is known about western European surgery during the early medieval period. The church, which controlled most aspects of social and political life, also tried to provide medical and surgical services. Ancient surgical knowledge was first introduced in the 11th century, when Latin translations of Arabic works were written in Italy and Spain.
Constantine the African was the earliest and most renowned of the translators. His work, which was accomplished at the monastery of Monte Cassino near Naples, Italy, stimulated the development of the nearby medical community at Salerno. Several surgical works were produced by the Salernitan school during the 12th century. The manuscript called the Bamberg Surgery, written about the middle of the 12th century and later found in a library in Bamberg, Germany, contains a formula for a “soporific sponge,” which consisted of opium, mandragora (mandrake root), and other ingredients to reduce the patient’s pain during an operation. The surgical text of Roger (Ruggiero Frugardi) mentions suturing the intestine over a hollow tube and treating an exposed intestinal wound by applying the moist intestines of a freshly killed animal. The wet, or open, treatment of wounds, which involved the intentional stimulation of pus formation, is associated with Salernitan surgery. The notion that such pus formation is desirable, which was the origin of the term “laudable pus,” remained in favor with a majority of surgeons until the 19th century. Roger’s text was copied, commented on, and elaborated by his student Roland of Parma and others.
Source . wikipedia.org
In the 13th and 14th centuries surgical texts written by educated authors became more plentiful. These men were associated with the early European universities—Bologna, Montpellier, and Paris. As university scholars, they were clergymen and doctors who wrote in Latin. Unlike the majority of their medical colleagues, they did not disdain writing about or even practicing surgery. But these men were few in number, and surgical practice was generally left to barbers and other uneducated workers. The educational and social gap between physicians and most practicing surgeons became wider as the universities developed during the late Middle Ages and the Renaissance. Thus, these surgical authors, including Theodoric, William of Saliceto, Lanfranc, Henri de Mondeville, and Guy de Chauliac, should not be considered representative of the surgical profession. They were acutely aware of the low status of surgery as it then existed, and they urged the recognition of its importance, the need for its improvement, and the need to link it more closely with medicine.
The surgical text of Theodoric, who lived during the 13th century and was associated with the university at Bologna, was based on the teachings of his master Hugh of Lucca. The dry treatment of wounds, which involved bringing the edges of the wound together, and the use of simple dressings were advocated over the Salernitan doctrine. The theory of surgery stressed at Bologna retained many of the features of Arabic medicine, including the preference of cauterization over the knife, bandaging rather than suturing, and the use of drugs in various combinations.
William of Saliceto, who taught at Bologna, wrote a comprehensive surgical text around 1275. He revived the use of the scalpel, stressed the importance of anatomical knowledge for the surgeon, and included case histories of his own patients. His pupil Lanfranc was forced to leave Italy because of his political involvements, and when he arrived in Paris toward the end of the 13th century he taught surgery in the faculty of medicine of the University of Paris. Lanfranc also gave lessons to the guild of Paris surgeons, which had formed during the middle of the 13th century. This surgical group, known as the confraternity of St. Come, persisted into the 17th century as a small group of learned surgeons. At the time of Lanfranc, and to some extent as a result of his work, surgical leadership in Europe passed from Italy to France.
The two outstanding French surgeons of the 14th century were Henri de Mondeville and Guy de Chauliac. Both of these men studied in Italy as well as at Montpellier and at Paris. Also, they were both doctors of medicine who practiced surgery and deplored the separation of the two professions. Henri de Mondeville was surgeon to several kings of France, and Guy de Chauliac served the popes during their residence at Avignon. The surgical text of Henri de Mondeville, written during the early 14th century, was never completed. In it, he questioned the prevailing devotion to the authority of Galen and the Arabic authors. He also opposed the open treatment of wounds and the use of complicated mixtures of drugs.
Guy de Chauliac’s famous work, Chirurgia Magna ( The Great Surgery ), was written around 1360 and remained the major surgical text until the 16th century. Abridgments in the form of catechisms for surgical students were published under Chauliac’s name as late as the 18th century. Although Chauliac was more conservative in style and content than Mondeville, ne was clear and methodical. He also stressed studying cadavers in preference to books.
Renaissance and 17th Century.
The fall of Constantinople to the Turks in the middle of the 15th century sent many Greek scholars to the West, particularly to Italy. Classical Greek medical works, which had generally been available in faulty translations from Arabic versions, were now translated directly from Greek into Latin. In addition, outstanding surgical works of antiquity, such as those of Paul of Aegina and Celsus, were rediscovered. About the same time the introduction of printing revolutionized the spread of knowledge. By the beginning of the 16th century, not only had costly editions of the works of Hippocrates and Celsus been printed but there were also inexpensive manuals available to surgical students. Although Latin remained the common language of the European scholarly community, an increasing number of surgical works were published in the vernacular for the benefit of artisans.
The emergence of strong secular states in Italy during the Rennaissance and the emergence of the nation-state in France, Holland, and England in the 16th and 17th centuries were accompanied by a lessening, if not the overthrow, of papal authority in those countries. Religious prohibitions on anatomical dissections and surgical operations were weakened. At the same time, warfare increasingly became the hallmark of European national policy, and the use of firearms permitted more complex fighting and caused more severe and different types of wounds. Skilled surgeons became indispensable to an effective army, and most of the outstanding surgeons of this period, as well as many of the less renowned, gained valuable experience as military surgeons.
The voyages of exploration and the development of overseas commerce required naval medical personnel, and, as in the army, most of these individuals were surgeons. Syphilis was Europe’s major new disease, probably introduced by the early explorers returning from the Americas. The treatment of syphilis, which consisted of applications of mercury, was a lucrative part of the practice of many surgeons.
Human anatomical dissection, which had been revived by Mondino of Bologna in the early 14th century, received great impetus during the Renaissance. In Italy, anatomical investigation and naturalism in art were combined by Leonardo da Vinci and others. The publication in 1543 of a magnificently illustrated text, Fabrica, by Andreas Vesalius, the professor of anatomy at Padua, led to the overthrow of Galenic doctrine in the field of anatomy. Abridgements of this text were used by surgical students as well as non-university practitioners.
Studies of anatomical changes caused by disease lagged behind the growth of the study of normal anatomy. However, in the late 15th century the Florentine surgeon Antonio Benivieni described pathological changes in more than 100 cases he had studied.
Except in Italy, and later in Holland, surgeons were excluded from the European universities. In 16th century Paris, the surgeons’ confraternity of St. Come received royal support but was unable to achieve its goal of university status. Most of the leading Paris surgeons of the 16th and 17th centuries came from the ranks of the barber surgeons, to whom the small group of educated surgeons left such tasks as bloodletting and the treatment of bruises, abscesses, and minor wounds. In the middle of the 17th century, the barber surgeons of Paris were legally united with the scholarly surgeons, and all university pretensions and forms of equality with the physicians were stripped away from the surgical community. From the modern point of view, the combination of the functions of the barber surgeons and the surgeons seems degrading to the surgeons. But prior to the 18th century, the status of the barber surgeon was not to be scorned. Nor was membership in a guild of artisans considered inferior, at least in economic terms, to association with a university. The barber surgeons performed their tasks adequately at a time when the physicians of the University of Paris were being ridiculed by the French dramatist Molière for their scholarly pretensions and their reactionary medical theories.
In other French cities and in the countryside barber surgeons took charge of most medical as well as surgical ailments. Similar conditions existed in the German state and in England, where the United Company of Barber Surgeons of London was formed in the middle of the 16th century. Major operative procedures, including the extraction of urinary bladder stones, cataract couching (moving the lens of the eye), and amputations, were usually performed by traveling empirics, men who had received no formal training but relied on their experience. Frequently, a family would develop a specific operation, technique, or even an instrument and transmit the secret knowledge from one generation to the next. In Italy, the Branca family specialized in plastic surgery of the nose, and the Norsini family specialized in hernia operations. The Colots were a French family specializing in the remov»l of urinary bladder stones, and the Chamberlens, a French-English dynasty, devised the obstetrical forceps.
France continued its surgical leadership during the 16th and 17th centuries, and the career of Ambroise Paré, the most famous surgeon of the Renaissance, illustrates many aspects of this period. Paré, the son of a poor provincial artisan, served his apprenticeship under a Paris barber surgeon. As a student barber surgeon he worked for three years in a large Paris hospital, the Hotel Dieu, where he was able to perform autopsies and dissections. Paré then began a long career as a military surgeon, finally attaining the post of first surgeon to successive kings of France. The confraternity of St. Come acknowledged Paré’s stature by seeking his membership and by relaxing the usual scholarly prerequisites for admission. Paré enhanced the prestige of surgery by the example of his career, by his writings, which were in French and stimulated the publication of other treatises in the vernacular, and by his reputation for integrity and humanitarian concern for his patients.
Paré relied heavily on his own experiences and observations and made several fundamental contributions to the development of new techniques. His chance discovery that gunshot wounds heal better when treated without the customary application of boiling oil led him to oppose the prevailing doctrine that such wounds were always poisonous. He was also among the first to control bleeding by ligating (tying off) arteries during an amputation rather than by applying the hot cautery iron. Paré also contributed to the field of obstetrics, although ordinary deliveries for women of all social classes were performed by midwives until well into the 18th century.
Pierre Franco, a contemporary and fellow countryman of Paré, came from even humbler origins. Franco, who worked in various places in France and Switzerland, condemned the ignorance and dishonesty that he observed among the itinerant “cutters.” Although he did not achieve a reputation comparable to Paré’s, he appears to have been a bolder and more ingenious surgeon. His descriptions of operations for strangulated hernias and the extraction of urinary bladder stones are still considered masterful.
In the German-speaking lands, surgeons of the late 15th and early 16th centuries began writing treatises in German on the treatment of battle wounds and amputation techniques. Wurtz of Switzerland excelled in these procedures, and Fabricius of Hilden, the leading German surgeon of the late 16th and early 17th centuries, was a bold original thinker who discarded the ancient concepts of pathology still followed by his contemporaries, including Paré.
Richard Wiseman, whose career as a military surgeon and eventually as surgeon to King Charles II is reminiscent of Paré’s, was the preeminent figure in 17th century British surgery. In Italy, Gasparo Tagliacozzi refined plastic surgery, particularly the restoration of the nose by skin grafting. At Padua, the tradition of Italian university surgeon-anatomists was furthered by the work and teaching of Fabricius ab Aquapendente.
18th Century.
During the 18th century the social status of the surgical profession improved markedly. As surgeons ended their association with barbers they approached social equality with physicians. A liberal education, followed by public and private courses in anatomy, surgical operations, physiology, pharmacy, and other subjects, began to supplement the traditional practical surgical training of apprenticeship, hospital work, and military experience. AJjhough there were few completely new operations devised, better methods and instruments for traditional operations were developed and refined. Hernia operations, eye surgery, and bladder stone operations passed from the hands of quacks into those of regular surgeons. Less encumbered than their medical colleagues by obsolete theories, the surgeons related autopsy findings to the clinical course of disease and made some progress in the experimental approach to disease and surgical therapy.
The leading surgical centers during the first half of the 18th century were Amsterdam, Leiden, and Paris. Starting about the middle of the century, London surgery advanced rapidly. Throughout Europe scientific societies flourished in major provincial cities as well as capitals. These societies published memoirs, conducted extensive correspondence, and awarded prizes for essays on scientific problems. In contrast to the universities, which generally continued to exclude surgeons, the societies accepted them and treated them as scientific equals with physicians. The sections devoted to anatomy in society publications included many outstanding surgical articles. The growth of other medical periodicals, their numerous translations, and the mobility of students also facilitated the exchange and spread of surgical knowledge throughout Europe.
The trends in surgery during the 18th century are illustrated in the following story about Frère Jacques ‘ (Jacques de Beaulieu ), who appeared in Paris in 1697 with a new and initially successful method for operating to remove urinary bladder stones. His ignorance of anatomy was revealed by a surgeon-anatomist of the Academy of Sciences who had been commissioned to dissect the cadavers of many of Frère Jacques’ patients. However, even the strongest of his critics thought that his technique had advantages that could be used by a competent surgeon with knowledge of anatomy. In 1704, Frère Jacques went to Holland to teach his technique to the Amsterdam surgeon Johann Jacob Rau, who improved it and refined the instruments. In the 1720’s, William Cheselden, a famous London surgeon and member of the Royal Society of London, adopted the method and improved it further. Finally, in 1729, the Paris surgeon François Sauveur Morand was sent to London by the Academy of Sciences to learn Cheselden’s technique. Morand reintroduced the method into Paris at the same time that several Paris surgeons were independently demonstrating its value. During the rest of the 18th century, this technique was the preferred method for bladder stone removal, even though a variety of alternate procedures and instruments were devised.
Procedures for amputations also were improved in the 18th century. English, French, and Dutch surgeons in the late 17th and early 18th centuries mastered the techniques of separating a limb at the joint and the application of skin flaps to the stump. Operations on the head, chest, and abdomen were generally avoided, but French surgeons could successfully remove segments of the intestines that had become gangrenous as a result of a hernia. And when a patient’s life was endangered, deep-lying abscesses and other collections of fluids were incised and drained. Considerable progress was made in the description and treatment of orthopedic disorders, such as fracture of the clavicle and tearing of the Achilles tendon. New instruments were devised for treating diseases of the urinary system and for removing or cutting off the blood supply to abnormal growths inside body openings. Arterial aneurysms (swellings) in the extremities, which had formerly been untreated or treated by amputation of the limb, were cured by ligating (tying off) the affected artery. The first correct pathological description of eye cataracts was published in the first decade of the 18th century, and around the middle of the century the modern operation for the extraction of cataracts was devised.
The leading surgeons of the capital cities of Europe were skilled in most, and often all, of these procedures, but they were still a relatively small group, numbering perhaps between 50 and 100 in Paris, the leading center. The expansion of the hospitals, both in number and size, stimulated the growth of surgery. Hospitals employing the foremost surgeons increasingly became the focal points for the practice and teaching of surgery, and advanced surgical students received room and board in the hospitals. Similar developments did not occur in medicine until the early 19th century. However, most surgeons continued to practice bloodletting and to treat wounds, ulcers, abscesses, and a variety of minor medical diseases in their shops or in the patient’s home.
The progress of the surgical profession in France was greatly supported by the royal government. The chief surgeons of the king-Georges Mareschal, François de la Peyronie, and Pierre de la Martinière—were also leaders of the surgical communities in Paris and the provinces. They used their influence with the government to obtain legislation and financial support. They used their influence over the surgeons to put their reforms into effect. Within a 20-year period, from 1724 through 1743, a royal college of surgery was established in Paris, educational requirements for surgeons were raised, and the surgeons were finally separated from the barbers. The formation of the Royal Academy of Surgery in Paris in 1731 profoundly influenced surgery not only in Paris but throughout France and the rest of Europe.
The leading Paris surgeon of the first half of the 18th century was Jean Louis Petit, who studied blood clotting and devised a tourniquet to control bleeding. His writings dealt with a wide range of surgically treated diseases, operations, and instruments. Toward the end of the century, French surgery was dominated by Pierre Joseph Desault, the chief surgeon of the Hôtel Dieu. Although Desault published very little, his work was made known by his students, the most famous of whom was Xavier Bichat. Desault was a conservative surgeon, who avoided amputation whenever possible and popularized bloodless methods (using elastic tubes) for removing obstructions from the urinary passages and esophagus. Desault’s main contributions were in the fields of blood vessel surgery, orthopedics, and diseases of the urinary system.
William Cheselden, the outstanding London surgeon and anatomist of the first half of the 18th century, was famous for his dexterity and speed in extracting bladder stones. He was also well known for his construction of an artificial pupil that restored the sight of a blind child. Cheselden began a tradition of high quality teaching among London hospital surgeons, and he was influential in securing the separation of the surgeons from the barbers by Parliament in 1745. Percival Pott succeeded Cheselden as the most prestigious London surgeon in the second half of the century. Another London surgeon, John Hunter, was a pioneer in the experimental approach to an understanding of normal function and disease. From his studies on the circulation of the blood in animals, he devised a procedure for operating on aneurysms.
The German-speaking countries lagged behind France and England during the 18th century. While barber surgeons continued to flourish, most university professors of surgery wrote about operations that they did not personally practice. In Germany the educational gap between the physician and the surgeon persisted, though it had been eliminated by mid-century in Paris and by 1800 in London. Only a few individuals, including Lorenz Heister and August Gottlieb Richter, were outstanding teachers, authors, and practitioners.
In Italy, surgery continued to hold a respectable place in the universities. Antonio Scarpa, a professor at Pavia, published beautifully illustrated texts on surgical anatomy.
19th Century.
In France, in 1794, the Revolutionary convention established new medical institutions, the Écoles de Santé, which united the teaching of medicine and surgery. All students were to receive the same theoretical and practical training, with slight variations in the final year depending on whether they wished to become physicians or surgeons. In England, medicine and surgery remained separated institutionally, but the creation of the Royal College of Surgeons in 1800 was evidence of the social and intellectual equality of the two professions. Several German teaching institutions, such as the Josephium in Vienna, combined the teaching of medicine and surgery. In the United States, rigid separation of the two professions had never developed.
Progress in surgery was gradual and unspectacular during the early 19th century. The Napoleonic Wars brought improvements in wound treatment and amputation. Pierre Percy and Dominique Larrey, distinguished French military surgeons, instituted methods of bringing prompt care to wounded soldiers. Guillaume Dupuytren, the leader of Paris surgery from 1815 to 1835, studied pathological anatomy. In London, pupils of John Hunter, including Astley Cooper and John Abernethy, carried on Hunter’s tradition of experimentation, as did Philip Syng Physick in Philadelphia. Two other American surgeons, Ephraim McDowell and J. Marion Sims, were pioneers in the field of gynecological surgery.
In 1846 the first major operation with the anesthetic ether was performed in the Massachusetts General Hospital. A dentist, William Morton, had persuaded Boston surgeons to try his sleep-inducing pain-killer. Morton’s success was dramatic and well published, and within a short time anesthesia was adopted by leading surgeons throughout Europe. Excruciating procedures, such as the reduction of fractures, could now be done painlessly, and organs that had rarely been operated on, particularly the abdominal organs, could now be treated surgically. The time available for operating was greatly increased, and surgeons no longer had to steel themselves to agonizing cries of patients or to worry about the patient overcoming the restraint of cords and assistants. To a considerable extent, the patient’s fear of operations was also removed.
However, anesthesia was not an unmixed blessing. The time limit for an operation was restricted to about an hour, and an operation could be interrupted by too light or too heavy doses of anesthetic. Even more seriously, bolder surgical operations led to a marked increase in deaths after apparently successful operations. Those surgeons who followed relatively sanitary procedures, like the British surgeon Lawson Tait, or those who operated outside the hospitals achieved better results. Some improvement was made by using instruments, rather than the hands, for clamping severed blood vessels and by the draining of abdominal wounds. But surgeons were unaware of the relationship between microorganisms and infectious disease and were unable to deal with the alarming rise in fatal postoperative wound infections. It was unthinkable to most surgeons that they themselves were contaminating their patients’ wounds.
In the 1840’s the medical profession rejected the observation by Oliver Wendell Holmes that the occurrence of puerperal, or childbed, fever was related to the uncleanliness of the obstetrician. A few years later, Ignaz Philipp Semmel-weis, an obstetrician in Vienna, realized that puerperal fever is a contagious disease similar to a wound infection. His statistical studies, which were published in 1861, clearly showed that women became infected during childbirth by contact with unclean material usually carried on the hands of the obstetrician. In spite of the fact that Semmelweis had been able to eliminate puerperal fever among his patients by instituting « sanitary measures, chief of which was the washing of his hands in a disinfectant solution, the medical community actively opposed his conclusions.
The work of the French chemist Louis Pasteur in the 1850’s and later led to the eventual widespread adoption of the germ theory of disease. Joseph Lister, professor of surgery at Glasgow, learned of Pasteur’s studies of fermentation in 1864 and realized that microorganisms might also cause tissue breakdown and pus formation, just as microbial ferments brought about the decomposition studied by Pasteur. This would explain why compound fractures, which were exposed to the air and thus exposed to harmful germs, became infected, whereas simple, or closed, fractures did not. Lister reasoned that the elimination of germs from a surgical wound would stop infection, and he attempted to achieve this antiseptic effect by placing dressings soaked in a solution of carbolic acid (phenol) over the wound. Later, Lister applied the carbolic acid to sutures and instruments and even sprayed the operating room with it. Lister’s first paper on antisepsis, published in 1867, reported the successful treatment of open fractures without the pus formation that most surgeons had come to accept as unavoidable or necessary. Despite Lister’s increasing success, many of his fellow surgeons were opposed to his ideas. German surgeons were among the first to adopt his method of antisepsis, and finally, by about 1875, it was generally accepted.
Antisepsis was unquestionably one of the most important advances in the history of surgery. The use of carbolic acid, however, was somewhat unsatisfactory because of the acid’s caustic nature. In 1878, Pasteur suggested the sterilization of surgical instruments and other materials by heating them. This method is known as asepsis. In antiseptic surgery, germs in a wound are destroyed by chemical agents. In aseptic surgery, the aim is to remove germs from everything contacting the patient’s skin or wound. Asepsis was adopted in the mid-1880’s by the French surgeons Terrilon and Terrier and by the German surgeon Ernst von Bergmann. By 1890 it was generally preferred to antisepsis. The introduction of sterile rubber gloves by the American surgeon William S. Halsted in 1885 and the later introduction of the sterile cap, mask, and sheets furthered the development of aseptic surgery.
By the last quarter of the 19th century, Germanic cities, particularly Berlin and Vienna, had become the world’s leading centers for surgery. In Vienna, Theodor Billroth and his colleagues and students performed the first operations for cancer of various gastrointestinal organs. The Billroth clinic also expanded experimental surgery and the microscopic study of diseased tissue. Theodor Kocher, a Swiss surgeon, operated on the thyroid gland as a treatment of goiter in the 1880’s. He also discovered the nature of the thyroid gland and many of its various functions.
Eduardo Bassini, at Pavia, Italy, devised the modern operation for the repair of an inguinal hernia in the late 1880’s, and in London, Victor Horsley pioneered in the field of surgery on the nervous system. In the United States, Halsted contributed to thyroid, breast, hernia, and blood vessel operations. He devised new surgical instruments, suture materials, and techniques of hemostasis (control of bleeding) and tissue handling during operations.
20th Century.
To a large extent, 20th century surgery has been concerned with making the operations developed during the 19th century safer. This progress has been aided by the close cooperation between surgery and the rapidly developing fields of physiology, biochemistry, genetics, immunochemistry, and other branches of science.
The discovery of X-rays by the German physicist Wilhelm Konrad Roentgen in 1895 soon led to the use of X-rays as invaluable diagnostic tools for both medicine and surgery. In 1900 the Austrian pathologist Karl Landsteiner distinguished the basic blood groups in man, and blood transfusions, which had been attempted sporadically since the 17th century, often with disastrous results, became feasible. Improvements in blood storage and transfusion made after World War I permitted the routine performance of operations that had previously been avoided because of the high risk of the patient hemorrhaging and going into shock.
World War I turned the surgeon’s attention from spectacular new operations back to the fundamental problems of wound treatment. Despite antisepsis, the mortality rates from wound infections were appalling. Although the antibiotic penicillin was discovered by the British bacteriologist Alexander Fleming in 1929, his work was at first ignored and it was not until the beginning of World War II that penicillin was produced on a large scale. Meanwhile, army surgeons learned that the removal of dead tissue and foreign material, followed by the open treatment of wounds, achieved better results than the immediate closing of the wound.
Much was learned in the field of neurosurgery from the injuries suffered by soldiers in World War I. Harvey Cushing of Boston was the leader in brain surgery and surgery of the endocrine glands. Cushing’s laboratory studies on animals enabled him to correlate experimentally induced disorders with many conditions in his patients.
During the period between the two world wars, improvements in anesthesia permitted much longer operations, and anesthesiology became a medical specialty, not simply a task relegated to junior surgeons or hospital attendants. Many other specialties became well defined during this period. Scientific as well as economic world leadership passed from Germany to the United States, where many physicians returned from military service with experience in surgery and the desire to pursue a specialty. In 1937 the American Board of Surgery was formed to set standards for training and practice. Residency programs modeled on Halsted’s at Johns Hopkins University were established at many universities.
The period following World War II has seen the increasing development of surgical clinics with facilities for all specialties. Laboratories in which surgical techniques are tested and physiological problems are studied have become prominent features of university surgical departments.
mavi